by
John R. Fischer, Senior Reporter | March 01, 2019
A new test is capable of assessing
the flow of blood to determine if the
source of their pain is cardiac-related
Predicting which patients require cardiac catheterization is now easier for clinicians at the Yale School of Medicine.
The Ivy League med school is the first in Connecticut and one of a handful in the Northeast to try out a new, personalized cardiac test for examining blood flow to the heart, to accurately predict appropriate candidates for catheterization among patients with coronary artery disease at Yale New Haven Hospital.
“This new analysis is helping us develop the most appropriate treatment plan for a patient with coronary artery disease (CAD) without the need for unnecessary and stressful procedures,” said Dr. Hamid Mojibian, M.D., associate professor of radiology and cardiology at Yale School of Medicine, in a statement.



Ad Statistics
Times Displayed: 174127
Times Visited: 3177 For those who need to move fast and expand clinical capabilities -- and would love new equipment -- the uCT 550 Advance offers a new fully configured 80-slice CT in up to 2 weeks with routine maintenance and parts and Software Upgrades for Life™ included.
Current exams for assessing blood vessels and the heart are prone to false positives, especially in women.
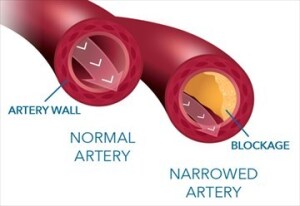
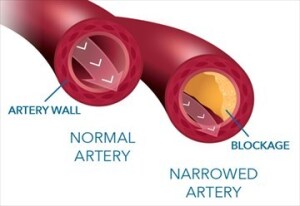
Relying on algorithms to simulate blood flow and assess the impact of narrowed vessels on flow to the heart, the test collects data from a noninvasive coronary CT angiogram of the patient and compiles an analysis.
Based on this, it then creates a personalized, digital 3D model of the blood vessels, the use of which was found to identify which patients were in need of invasive treatment versus those that were not, in clinical trials.
One example is the case of a 73-year-old with multiple medical conditions that made the cause of chest pain he was feeling unclear. Following the completion of a coronary CT angiogram, the test found no significant arterial blockage of blood flow to the heart, ruling out cardiac as the source of the pain.
Its use, according to Mojibian, will help patients who do not require catheterization avoid unnecessary invasive angiography, a practice that patients with chest pain and shortness of breath often choose to undergo. A recent study from the New England Journal of Medicine asserts that such procedures are not necessary in many cases, finding no CAD in 39.2 percent of patients who received catheterization.
“This new analysis is helping us develop the most appropriate treatment plan for a patient with coronary artery disease (CAD) without the need for unnecessary and stressful procedures,” he said. “If 40 percent of diagnostic catheterizations in this situation are normal, we can use this new tool to make sure the right patients are getting cardiac catheterization as quickly as possible. We can reduce the number of false positives, thereby avoiding unnecessary catheterization, reducing complications, providing value and creating faster diagnosis.”
Back to HCB News